When I think of Alzheimer's, I don't think of somebody like Daniel Gibbs. I think of my mother, who doesn't know what year it is, or that her husband is dead. I think of tragic movie characters in tearjerker films.
Gibbs would like to change that. As a neurologist, he understands the science of the brain. As an early stage Alzheimer's patient, he recognizes there is so much more to the condition than the singular — and extreme — narrative we may be familiar with.
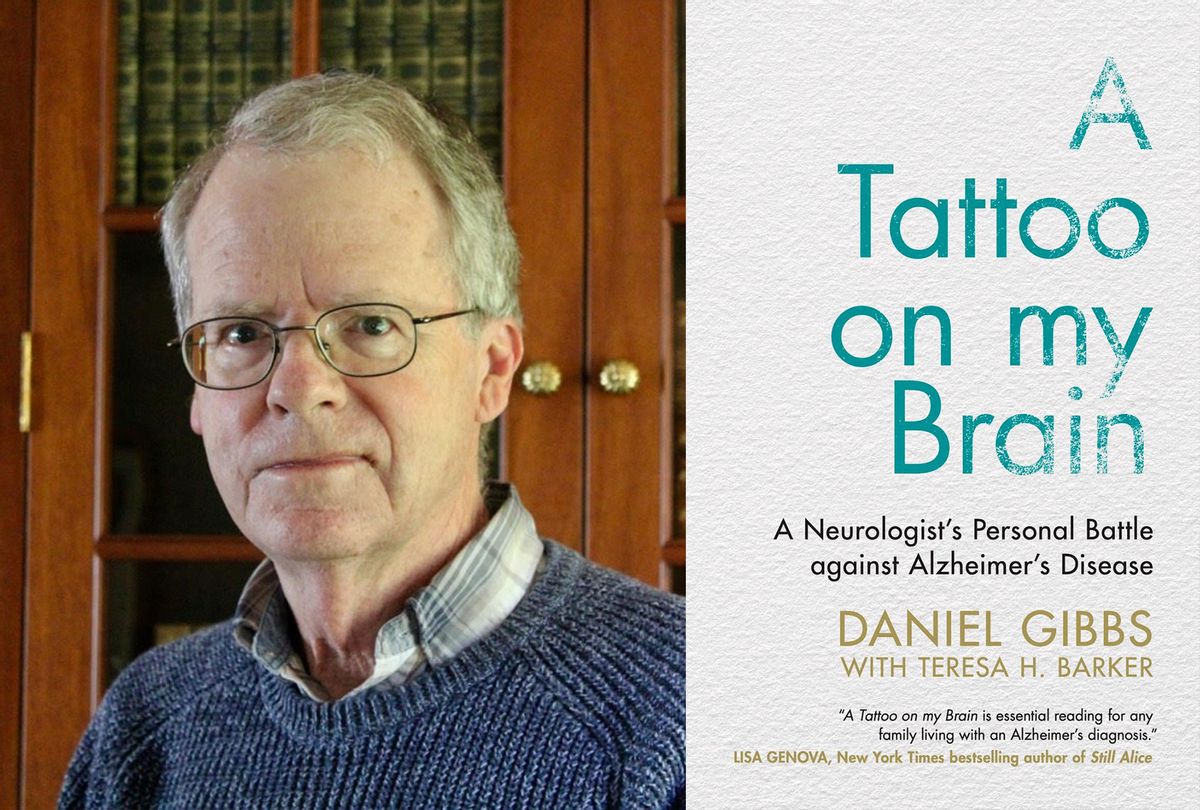
In "A Tattoo on My Brain," co-written by Teresa H. Baker, Gibbs reveals how a surprise diagnosis changed his life, and how modern Alzheimer's doesn't have to be the confounding "senility" of generations past. With equal parts humility and curiosity, he offers a firsthand account of a disease that affects 5.8 million Americans, and for which there is no cure. And he investigates the new thinking and clinical research that's offering hope to patients like him, as well as people like me, who wonder what might lurk in our own genetic future.
Salon spoke to Gibbs recently about the myths of misconceptions of Alzheimer's, and how his sense of smell tipped him off to a bigger problem. As always, this interview has been condensed and edited for clarity.
In your book, you call yourself a "lumper." What do you want people to understand about Alzheimer's, about dementia, all of those things that we "lump" together?
There's a parallel with cancer because Alzheimer's research is about thirty or forty years behind our understanding of cancer. Back in the fifties and sixties, cancer was just all thought to be about the same — the cells went wrong and grew, and if you could kill one cancer, you might be able to kill them all. Obviously, that wasn't true. Alzheimer's has been following the same path. When I was first in practice, we couldn't do anything about any of the dementias. I lumped them together because it didn't seem to be fruitful to make a distinction between Alzheimer's disease and Lewy body dementia or Parkinson's dementia or vascular dementia, frontotemporal dementia.
When the first drug, Aricept, came out in the nineties, it became important — for me anyway— to make a distinction, because Aricept provides some benefits to some people with Alzheimer's, some people Lewy body dementia. But it can make symptoms from frontotemporal dementia actually worse. It was important to get rid of the shotgun approach and more fine tune.
Just in the last year, in the last few months, we're finding that there are probably subtypes of what we call Alzheimer's that really aren't quite the same thing on a molecular level. They probably will respond or not respond differently to various attempts to reverse the disease or to slow it down.
That's become apparent in the trials of disease modifying medications, like the anti-amyloid monoclonal antibodies, the trial that I was in. Early on the trials of the first drug, showed absolutely no benefit. But in those first trials, they weren't able to test to see if people actually had Alzheimer's disease. That was before the amyloid pet scan was available. Now, all of the trials require a pet scans for amyloids, to show that the people all have these amyloids in their brain. It doesn't mean they have Alzheimer's disease, but it means that they are probably on the path.
My feeling is we're going to have to push the target age earlier, working on treatments even before people have cognitive impairment. It's not as simple as one type of cancer; it's probably not one simple type of Alzheimer's disease. We have to understand more about the different subtypes before we figure out how to attack it.
That's crucial, because a lot of us have a particular narrative in our heads about what it looks like when someone has Alzheimer's. Anthony Hopkins and Julianne Moore have won Oscars for it. Yet you start your story with very different symptoms, that we don't necessarily recognize as being part of Alzheimer's.
I started to lose my sense of smell at least fifteen years ago, and didn't think anything of it because everybody, as they get older has a decrease in their sense of smell. But about a year into it, I started to have weird, illusory odors, which incidentally are not the characteristics of Alzheimer's disease. That there's nothing in the literature that I could find that showed an association.
But that got my attention because that was weird to have these smells come out of nowhere that were a cross between baking bread and perfume, that would last a few minutes or maybe an hour. I was more interested to see if I might be at risk for Parkinson's disease, because olfactory disorders are much better recognized in Parkinson's. Alzheimer's wasn't on my radar screen at all.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter The Vulgar Scientist.
There are psychological symptoms that maybe someone who is looking at changes in their own behavior or mental state may not realize might be symptomatic. What was that like for you?
Apathy is so common. I think it's probably due to one of the first parts of the brain that starts to accumulate amyloid is the prefrontal cortex. That's the part of the brain right in the front that is involved in motivation. It's where we come up with plans for doing things. It just makes sense to me. That probably is the structural correlate of why we get apathy. I certainly have a hard time doing stuff. I'm content with the isolation of COVID and don't really have a particular interest in going out again now that I can go to the theater or something like that. I have to push myself to do that, or my wife has to push me.
That's very common and it's often very early. The things like the paranoia, the real psychiatric symptoms that can be so difficult for everybody, are usually later. Unfortunately I think what we've all considered to be Alzheimer's disease is that late stage. When I was practicing neurology, at least in the first ten or fifteen years, that was the first time I saw somebody with Alzheimer's. They wouldn't come to the doctor until those late stages, and there wasn't really anything to do back then. There still isn't much to do. And there probably won't be much to do for those people in terms of trying to reverse the process, because by that time brain cells are dead and we just don't have a clue how to bring them back.
The first successes in terms of disease modification, in my opinion, are going to be in the earliest stages of the disease, but probably before people have any symptoms and that's going to be really hard to manage.
Over the past year or so it has been harder for all of us to really assess our own mental and physical health, and that of our loved ones. Do you feel that this pandemic has had a detrimental effect on people who are vulnerable to Alzheimer's and people living with Alzheimer's?
I don't think that I can say that it's had a detrimental effect on me per se, but I think people who are living by themselves, it must be terrible if they have early Alzheimer's to have that additional isolation. We have four grandchildren, and for the last couple of months, we've been able to get together. I think the isolation has been really hard for the people who aren't able to interact in person with anybody.
For those of us who are in the caregiver roles or extended family member roles, who see this in our families, it's scary. What do you tell those of us who are either facing this diagnosis or worry that we're going to face it?
It's so important that we're able to come out of the closet with Alzheimer's because there's been this real stigma attached to it. People are afraid of people with Alzheimer's. They don't know how they interact with them, and there's a drawing back. I see that even from myself. The first reaction that people tend to have when I tell them that I have Alzheimer's, especially a few years ago, was, "Oh, no, of course you don't have Alzheimer's," because it doesn't fit the paradigm that people have in their mind of the image of what someone with Alzheimer's ought to look like. I make it a point to just lay it out there before people can be put off by it. Everybody in our neighborhood knows I have Alzheimer's, and I think that's good.
The people that might want less to talk about it, are older people, because it's maybe a little more threatening to them. Younger people are more open minded about it. I think that's really great because that's my target audience, especially if they have a family history of Alzheimer's because the biggest risk factor is a parent or a sibling with Alzheimer's. Those are the people who really need to start doing something about it when they're middle age or before. There's really good data that some of these lifestyle modifications that I go into in the book can reduce the risk of getting Alzheimer's when you're in your seventies or eighties. But they have to be started early.
If you wait until you're 70 and starting to have memory issues, the horses are out of the barn to certain extent. I's much more effective to start exercising regularly and eating well and getting sleep. There was a really good study that came out a few weeks ago that gave us the best data yet about how important it is to have adequate sleep in midlife. And that's the hardest time to get adequate sleep, because we're so busy. They found that that people who got six or less hours of sleep a night had a 30 percent greater risk of getting Alzheimer's than people who got seven or more hours of sleep at night. I go into some of that about sleep in the book about why that might be happening. The glymphatic circulation in the brain.
Tthe bottom line is it really does help, but it needs to be midlife. It doesn't help start trying to get a lot of sleep when you've already got Alzheimer's. By that time, it's really hard to get adequate sleep because Alzheimer's stalls up sleep patterns. It's got to be early, and that's going to be the case for the drugs that finally work to slow down or keep us from getting Alzheimer's. I think they're going to have to be used in people in their fifties, before they have any signs of disease, but that's a bit of a controversial assertion.
How do you feel about early genetic testing and testing if you don't have symptoms?
A reason to get tested would be, if you had a family history, and if you're interested in getting involved in a study. We're going to need thousands of people in that category, to have an impact on preclinical disease. I don't recommend that people go out and get tested for Alzheimer's without any structure. I think if you want to get tested that's okay, but it should be done under supervision so that somebody can explain what your risk really is.
That's going to get even more complicated within a few years, because I think we're just a few years from having really good blood tests for both amyloid and tau available that will really prove the diagnosis of pre symptomatic Alzheimer's disease.
If have a first degree relative without Alzheimer's, so then you ought to be out there getting 10,000 steps or running, getting your aerobic exercise every day, or at least three times a week at the very least. A lot of people don't enjoy or think don't think they enjoy the heart and brain healthy diets that are more plant-based, but that would be a good thing to at least make an effort to head towards. It's good for your heart, it's good for your blood pressure, it reduces risk of diabetes and it's good for your brain. I would recommend at least those modifications and trying to get some sleep and staying intellectually active. You don't have to know whether you've got the gene for it, or whether you've got tau or amyloid in your brain. At least for right now, just for those who have a family history, I would really recommend making the lifestyle modifications. It doesn't matter whether or not you know that you have a genetically disposition or already having amyloid.
I was thinking recently how much my fear of cancer has changed because of my dad dying at 60, when I was only 16. I've always been worried that I was going to have cancer. I was really dreading it. Now that I have Alzheimer's, my view of cancer is totally changed and I'm not afraid of cancer anymore. I'm hoping that the things I'm doing in my life to mitigate the effects of Alzheimer's will prolong my life, prolong my healthy brain part of life, for as long as it takes for something else to kill me. Because I don't want to die of Alzheimer's disease.
Shares