Since Alexander Fleming discovered the very first antibiotic, penicillin in 1928, antibiotics have become a revolutionary tool for fighting infectious diseases. For over 70 years, these drugs have greatly reduced illness and death and transformed medical care across the world.
Since Alexander Fleming discovered the very first antibiotic, penicillin in 1928, antibiotics have become a revolutionary tool for fighting infectious diseases. For over 70 years, these drugs have greatly reduced illness and death and transformed medical care across the world.
Today, antibiotics are still vital in many instances and beneficial when prescribed and taken correctly. However, their widespread overuse and misuse has led to the creation of infectious organisms that have become resistant to the drugs, fueling a rapid increase in antibiotic-resistant bacteria.
According to a recent report by the Centers for Disease Control And Prevention at least 2 million people become infected with bacteria ever year that is resistant to antibiotics, and at least 23,000 people die as a direct result of those infections or from conditions complicated by the antibiotic-resistant infection.
Those who are infected with antimicrobial-resistant organisms are more likely to suffer from their illness for longer durations, require lengthier hospital care and are more susceptible to death because of the infection. Hence, antibiotic resistance not only places an economic burden on our entire health system but is considered to be one of the world’s most critical public health threats.
So, how does bacteria become resistant?
A recent CDC report explains that when bacteria are exposed to antibiotics over a period of time, they start to learn how to outsmart the drugs. Every time a person takes antibiotics, sensitive good bacteria in the body are killed off but the resistant germs are left to grow and ultimately multiply, creating superbugs. This in turn, leads to limited treatment options and can cause further dangerous bacterial infections that pose higher risks to human health.
Steve Solomon, director of CDC’s Office of Antimicrobial Resistance, explained the phenomenon to AlterNet:
“We call it the antibiotic paradox: the more you use antibiotics, the less effective they become. Antibiotics were such a remarkable drug when they were first discovered. Back then, the feeling was that any side-effects would be minimal compared to the life-threatening infections that up to that time had never been treatable. Until the 1980s, new antibiotics were being developed very rapidly to combat resistant bacteria. However, progressively our thinking and mindset toward antibiotics changed. The medical profession became complacent and worried less about antibiotic resistance. In the back of our minds we believed there would always be a new antibiotic coming along to treat infections. Sadly, this wasn’t to be.
“In the last 10-15 years, the development of antibiotics has slowed down tremendously. That era of somewhat complacency and feeling that there would always be new treatments is now long in the past, with two recent antibiotic inventions showing signs of resistance within only a few years. The concern now is that someone will get an infection and there will be no drugs to treat the infection because antibiotics are resistant to everything. That is the nightmare scenario.”
In fact, evidence suggests we have now reached a state in which there soon may be no assurance that we can treat infections effectively. Common conditions like gonorrhea, strep throat, pneumonia and the fungus candida are now considered infectious threats because they are showing increasing resistance to the drugs used to treat them, even among people who are young with seemingly good immune systems.
Our hygiene-driven, drug-reliant culture that seeks instant relief has contributed to the growing problem, fueled by our tendency to self-medicate and demand drug treatment for infections that antibiotics simply cannot treat. Likewise, the medical profession’s willingness to overprescribe antibiotics to satisfy patients, often derived from a fear of lawsuits, has further contributed directly to resistant infections.
In the United States alone, one in every five visits to a pediatric healthcare provider resulted in a prescription for antibiotics, accounting for 50 million antibiotic prescriptions per year. It is estimated that 10 million antibiotic respiratory prescriptions annually are directed toward viral respiratory tract infections, which cannot be treated with antibiotics.
Yet, the fallacy that antibiotics can treat all infections lives on. This is despite the fact that medical research clearly illustrates that antibiotics can only cure bacterial infections, not viruses, which are responsible for the majority of illnesses: colds, influenza, runny noses, most bronchitis, most sore throats, most sinus infections and some ear infections. In truth, most infections subside on their own.
Harry A. Milman, consulting toxicologist and president of ToxNetwork.com elaborated further to AlterNet on the dangers of overprescribing drugs.
“When you take antibiotics for a virus, you’re literally taking the drug for nothing. Not only are you not helping your immune system, but you are also directly making other bugs resistant,” he said. “The body is a wonderful machine that can take of and can mend itself. Our bodies contain white blood cells that fight against infections. When we take antibiotics, we are supplementing our body’s normal way to fix itself. Without supplementing, the body heals itself—it just takes longer. Antibiotics may speed up this process, but then you place yourself at greater risks of other serious health problems.”
Solomon agrees. “The vast majority of common colds or upper respiratory infections are overwhelmingly caused by viruses, both in adults and children,” he said. “People ask for and doctors prescribe antibiotics for far too many of these viral conditions and so that really represents a tremendous amount of overuse for the typical patient. Some progress has been made, but more needs to be done to help patients and doctors understand those situations where people should not prescribe antibiotics, not just to prevent drug resistance, but to avoid the serious side-effects of drugs. You just never want to take medication you don’t want or need to be taking.”
Furthermore, people tend to ignore the potential physical risks associated with antibiotics, which can be fatal. Antibiotic adverse reactions are responsible for one in five emergency department visits with an additional 150,000 healthcare visits per year associated with antibiotic usage. Yet, as Dr. Soloman explains, society tends to overlook such serious consequences.
“Antibiotics like any other drugs do have side effects. Allergic reactions are the main reasons people show up in emergency rooms. Again, in our culture people underestimate these side effects,” he said. “Patients will go into a doctor’s office and ask for an antibiotic believing somehow that there is no risk involved. Obviously there is! We could never imagine a patient coming in and saying, ‘Please give me a powerful drug for heart disease. I’m not sure I even have it, but give it to me anyway,’ yet people do it with antibiotics anyway.”
Consequently, Dr. Milman says it is important to choose the correct antibiotic. “All bacteria comes in different types and therefore not all antibiotics are appropriate. Each type requires its own antibiotics,” he said. “So your treatment has to be bug-appropriate. Once you start medication, you should really take it as prescribed and take the full dosage because you want to make sure you kill all the bugs to prevent bacteria from growing again and multiplying. In such cases, the bacteria is now stronger and more resistant because it’s been subjected to a partial dosage of antibiotics and can now handle it. In effect, you have created a superbug. It’s basically survival of the fittest.”
This kind of misuse of antibiotics contributes to the development of resistant bacteria, according to Dr. Soloman. “In some cases, partial treatment or not finishing a dose, does encourage the development of resistant strains of bacteria. One of the reasons that finishing a course of antibiotics is so important is the risk of a relapse,” he said. “Doctors are concerned that if a patient feels better and decides not to finish the course, the bacteria is insufficiently wiped out, therefore putting the patient and others at risk of developing resistant bacteria. Clearly, if people wish to discontinue antibiotics because of an allergic reaction, they need to report back to their doctor and have an honest conversation about what is going on and figure out what is the best course of action to take.”
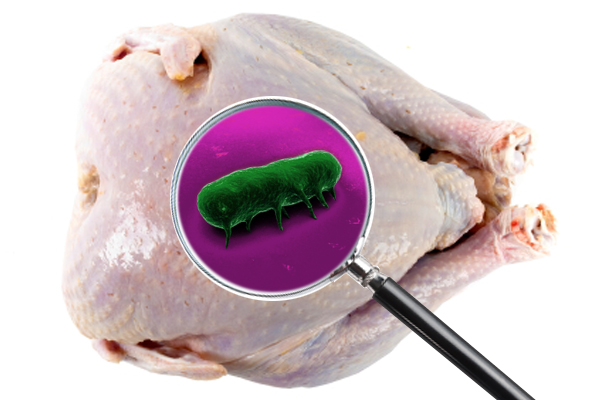
Other factors contributing to antibiotic resistance include the widespread use of antibiotics in agriculture, specifically on livestock in animal feed to stimulate growth and control disease due to the unhealthy, unhygienic and overcrowded conditions in which the animals are forced to live. This has become such a serious problem that the FDA recently announced new policies to curtail the widespread use of antibiotics on farms and phase out their use in animal growth because the drugs are starting to lose their effectiveness. In other words, the antibiotic resistant bacteria are spreading.
Anti-bacterial cleaning agents may also be adding fuel to the fire, rather than preventing the spread of bacterial infections. Concerns have surfaced that a key ingredient in anti-bacterial soaps, Triclosan, contributes to the emergence of drug-resistant germs, which causes antibiotics to become ineffective.
The FDA announced that there’s no evidence to suggest anti-bacterial chemicals are any more effective in preventing the spread of bacteria than plain soap and water. The agency will now require all manufacturers to prove that anti-bacterial soaps do not pose health risks or the products will have to be reformulated.
With so many rising obstacles, many in the public health industry have been left wondering why public funding is not being invested into creating new antibiotics. According to the CDC, most pharmaceutical companies, which are run by multinational corporations, are reluctant to invest in new antibiotic research because they’re concerned about maximizing return on their current drug investments.
Antibiotic research can cost anywhere between $ 800 million and $1.7 billion per drug, which is not exactly a venture that pharmaceutical companies are willing to take, particularly as the drug pipeline for most new drugs is shrinking and there is a lack of regulatory clarity from the FDA. The development process is not only costly but to ensure drugs are effective and safe, the testing procedures can go on for many years.
Such a bleak picture raises the question, are we coming to the end of an antibiotics era or is there a solution to this growing epidemic? Dr. Solomon is hopeful.
“Right now, we’re standing at the edge of the cliff. We’re at risk of going over that cliff and plunging right back to a pre-antibiotics era when infections can’t be treated. All of us—professionals, decision makers and the general public—have a decision to make,” he said. “We need to make the right choice, that being, to not act complacent about antibiotics and to implement a whole series of strategies. If we work harder to stop the spread of bacteria, increase our capacity to monitor the development and spread of bacteria, if we’re careful about the use of antibiotics and improve our stewardship of precious resources and if we encourage the development of new antibiotics by priming the pump, we are going to be OK.
“If we don’t do that, if we don’t take advantage of the knowledge we have to implement those practices in the future, we will go over that cliff and see more and more infections that can’t be treated. I am hopeful we can reverse the problem.”
Unquestionably, antibiotics are conducive as a medical solution to prevent serious infection following life-threatening surgery and other bacterial infections. However, it is important to remember that drugs aren’t always the answer and can be detrimental to the body’s own natural ability to fight infection. Sometimes, as CDC medical experts say, the safest prescription is to wait and see.
Here’s a list of antibiotic do’s and don’ts based on research tips from the CDC:
- DO get regular vaccinations against drug-resistant bacteria.
- DO implement good hygiene methods by washing hands before eating to prevent ingesting drug-resistant bacteria.
- DO cook meat and poultry thoroughly to kill bacteria.
- DO seek medical attention if you have an allergic reaction to antibiotics.
- DO follow the instructions about dose and duration.
- DON’T demand antibiotics when your doctor says you don’t need them.
- DON’T take antibiotics for viral infections.
- DON’T skip doses or take someone else’s antibiotics.