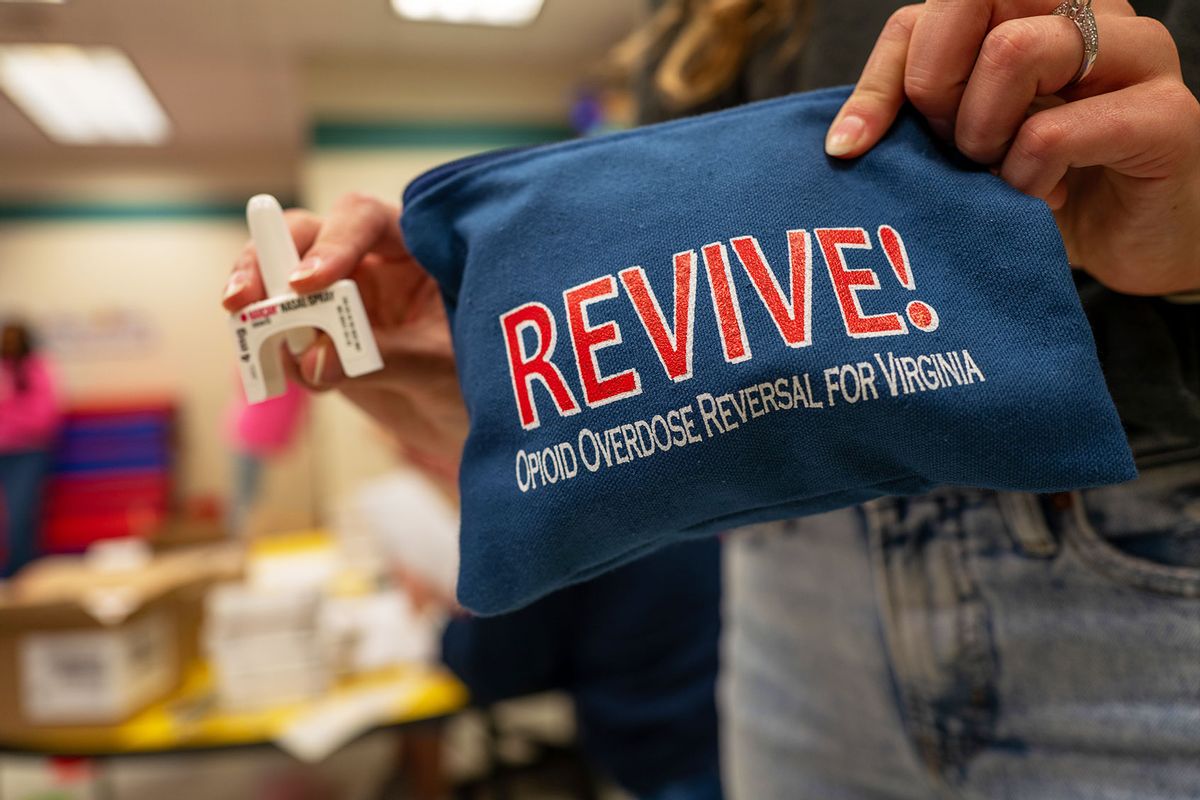
In recent years, several harm reduction interventions have been outsourced and integrated into the day-to-day work of various professions outside of harm reduction settings. One example includes police officers trained to administer naloxone to opioid overdose victims, since they are often the first on the scene after 911 is called.
However, research suggests that police officer views about people who use drugs are generally negative, and studies show that prior experience administering naloxone to an overdose victim is not associated with more positive views about this aspect of their jobs. Expecting a police officer to respond to an overdose may present a conflict for him within the broader context of the war on drugs. Law enforcement officers have been taught to see an overdose victim as a criminal who illegally acquired and used drugs from the underground market for half a century. Rather than viewing an overdose as a medical emergency, many have been trained to see it as evidence of criminal activity.
Yet we now instruct officers to look at the overdose victim as needing medical assistance and intervene with naloxone. And at the same time, we expect people who use illegal drugs to be willing to call 911 for help with the full knowledge that officers with the power to arrest them may be the first to respond. 911 Good Samaritan Laws were passed to protect overdose victims and bystanders from arrest when police officers respond to overdose calls. However, these laws have not significantly reduced overdose deaths because many people still fear arrest due to the limitations of state-specific protections in the Good Samaritan Laws and because many people still fear arrest.
The disconnect between the criminalization of drug use and our desire to promote a public health approach to the overdose crisis plays out in these situations every day. While it is important to ensure that any potential first responder, including a police officer, is prepared to help save a life and armed with naloxone, we must question whether police officers should be dispatched to overdose 911 calls at all. Why are police officers the first to the scene of a medical emergency rather than an EMT or another first responder with training in crisis response? What else could an emergency response look like?
Studies with pharmacists in several US states suggest that only a small percentage of them are willing to sell syringes without prescriptions and that many pharmacists hold negative and stigmatizing views of people who inject drugs.
Many harm reductionists support alternative crisis response hotlines which dispatch people trained in mental health and crisis response, like social workers and paramedics, to overdoses rather than police. More of these alternative hotlines are popping up in communities across the country, since it is clear how these trained responders would be better equipped to save lives, and vulnerable people may feel safer when calling for help. Harm reductionists also want public funds to prioritize buying and distributing naloxone for community distribution in higher quantities because families and friends respond to far more overdoses in our neighborhoods than law enforcement. Beyond this, harm reductionists continue to advocate for Overdose Prevention Centers so people can avoid calling 911 and get the help they need on site.
Another example that comes to mind is the provision of sterile syringes outside Syringe Service Programs (SSPs). Some states have passed laws so that you can legally buy syringes at the pharmacy without a prescription to increase access to sterile syringes for people who may not have an SSP nearby. In New York State – where most counties do not have an operational SSP – you can buy ten syringes without a prescription at any pharmacy through the Expanded Syringe Exchange Program (ESAP). By offering these services, pharmacies can fill this harm reduction gap in more parts of the state.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter Lab Notes.
However, there are limits to how much these programs can increase access to sterile syringes for the most marginalized people who use drugs. There’s often a large difference between what is legal and what happens in practice. Just because someone can legally sell syringes does not make their program a harm reduction program. And just because you can sell syringes to people who use drugs does not mean you will. Studies with pharmacists in several US states suggest that only a small percentage of them are willing to sell syringes without prescriptions and that many pharmacists hold negative and stigmatizing views of people who inject drugs.
I once guest lectured on harm reduction to a class of pharmacy students enrolled in the university’s PharmD program when I was an Assistant Professor of Social Work. Almost all of the students had current internships for school credit at community pharmacies across New York City and Long Island, so I asked them if they knew about the state’s ESAP law. Most of the students did not.
Think about how hard it must have been for these customers to walk through the door in the first place, given the stigma toward injection drug use and the fact that they “outed” themselves.
One student raised his hand and told me he recently had a customer come up to the counter to purchase syringes without a prescription but the managing pharmacist told him to lie and say they had no syringes in stock. Another student then raised her hand and said she had a similar experience; however, the managing pharmacist told her to tell the customer they only had large gauge syringes (intended for intramuscular injections) in stock, not the smaller hypodermic syringes the person had requested. In both cases, the customers left without the syringes they wanted.
I asked the class why they thought their classmates were discouraged from selling syringes. Some described a phenomenon known in the research as the “honeypot effect.” They believed that the managing pharmacists worried that selling syringes to people who used drugs would attract more of them to their pharmacies, particularly from other communities.
The students hypothesized that the pharmacists wanted to avoid serving these so-called undesirable customers and did not want to gain a reputation as a pharmacy that sold syringes to drug users because they wrongly believed it would invite more criminal activity to their neighborhood. Other students talked about how perhaps the pharmacists were worried about “enabling” or “encouraging” injection drug use by selling syringes.
I used these anecdotes as an opportunity for further discussion. First, I dispelled the honeypot theory by discussing existing research both in the United States and internationally that found that harm reduction programs of all types typically draw in only existing members of the neighborhood and do not increase crime in the vicinity of the program. I also encouraged them to think about how hard it must have been for these customers to walk through the door in the first place, given the stigma toward injection drug use and the fact that they “outed” themselves by making such a request.
I asked them how these customers must have felt when they were treated this way – did the students think the customers believed the staff when they said they had no syringes or only had certain ones, or did they know the pharmacy staff simply did not want to serve them? I asked them to imagine what happened when the customers left the pharmacy after being unable to buy those syringes. Would they try another pharmacy? Would they wake up the next day and simply stop injecting drugs because they had no new syringes? Would they reuse or share a syringe with someone else the next time, since they did not have sterile syringes of their own?
I also reminded the students that these customers came to the pharmacy fully intending to pay for these syringes. After all, SSPs give them out for free. So, if someone is coming to a pharmacy, they either have no nearby program or prefer the setting. By refusing to serve them, the pharmacists made it hard for these customers to engage in health-promoting behavior.
And they may have just discouraged these people from seeking syringes at a pharmacy ever again. I encouraged the students to think about what they would do if they were in this situation in the future. Would they behave differently? Many raised their hands when I asked whether they would consider selling syringes to customers.
We need your help to stay independent
I left that presentation thinking about the pervasiveness of drug-related stigma in our society and how much work it will take to get people to challenge their deep-seated thoughts and beliefs about people who use drugs. But it also reminded me that we cannot simply expect systems and institutions to be effective substitutes for harm reduction programs without adequate training and monitoring for compliance.
Of course, ESAP programs are reducing the spread of blood-borne infections, and police officers are reversing overdoses every day, and there are well-intentioned people who want to do it. But reviewing the research and reflecting on conversations like the one in my classroom also highlight exactly why harm reduction programs are still so essential and can never truly be replaced (at best, they could be supplemented by such approaches.)
Harm reduction programs clearly fill a gap in our communities because, unlike many parts of our healthcare system and criminal legal system, they not only welcome the highest-risk and most marginalized people in the door but also want them to be there.
Shares