Flu season is here and it’s already shaping up to be a pretty intense one. Illness is predicted to spread faster, infect more people and put higher-risk groups at greater chance of being seriously ill or hospitalized. Doctors and public health experts are warning people to take precautions, including getting this year’s flu shot.
For RNA viruses, such as influenza, survival is equivalent to replication. Every time the virus replicates in a host cell, it presents an opportunity for a mutation to emerge. While viruses are technically not alive, it is their nature to mutate and evolve. Through these mutations, they can become more contagious, evade immunity, and become deadlier. This past summer, as flu season cooled down in the Northern Hemisphere, it intensified in the Southern Hemisphere, giving influenza A (H3N2) another opportunity to mutate — and it did. According to scientists, seven mutations occurred, positioning the Northern Hemisphere to head into a rough flu season.
“This is a small group that emerged since June, and since it emerged, it’s rapidly spreading and predominating in some countries so far in the Northern Hemisphere,” Dr. Wenqing Zhang, head of the World Health Organization’s Global Respiratory Threats Unit, said in a media briefing this month, about the strain H3N2 subclade K.
Dr. Rajendram Rajnarayanan, of the New York Institute of Technology campus in Jonesboro, Arkansas, told Salon via email that the mutations “reshaped the areas that antibodies recognize,” making previous immunity, including immunity induced by the flu vaccine, less effective.
Specifically, Rajnarayanan said, this mutation’s significant antigenic drift, which is when the genes of a virus change, is “a real concern.”
“We have a narrow window to act — boost stockpiles, issue robust guidance, deploy resources quickly, and reinforce surveillance.”
“If you combine the immune escape from this drastic drift with further changes that boost viral fitness as it spreads more (which help the virus replicate better in human airways), you get a season where flu spreads faster, infects more people, and pushes high-risk groups into hospitals sooner, pushing infrastructure and capacity concerns,” Rajnarayanan said.
The signs are already here. In the U.K., Japan, and Canada, there have already been increases in flu cases, leading to an earlier-than-usual flu season. The UK Health Security Agency (UKHSA) data showed that flu-associated hospitalizations increased from the end of September into October, affecting people over the age of 75.
“Countries hit early may have been caught off guard and are scrambling to ramp up countermeasures,” Rajnarayanan said. “With early alerts now coming from our international partners, we have a narrow window to act — boost stockpiles, issue robust guidance, deploy resources quickly, and reinforce surveillance.”
Start your day with essential news from Salon.
Sign up for our free morning newsletter, Crash Course.
One concern is that this year’s flu vaccine was recommended before the new strain emerged. Fortunately, early studies show that the vaccine still offers some protection.
A recent study in the medical journal Eurosurveillance stated “our early estimates provide reassurance that current NH enhanced vaccines provide protection in children, adolescents and adults in the early period post-vaccination. The high VE [vaccine effectiveness] in children and adolescents strengthens the case for optimising vaccine uptake in this group, where we could also see indirect protection of other age cohorts.”
In England, the National Health Service issued a “flu jab SOS,” urging those eligible for the free vaccine to get it quickly and protect themselves this winter.
“I am concerned about everything related to infectious disease under the Trump administration.”
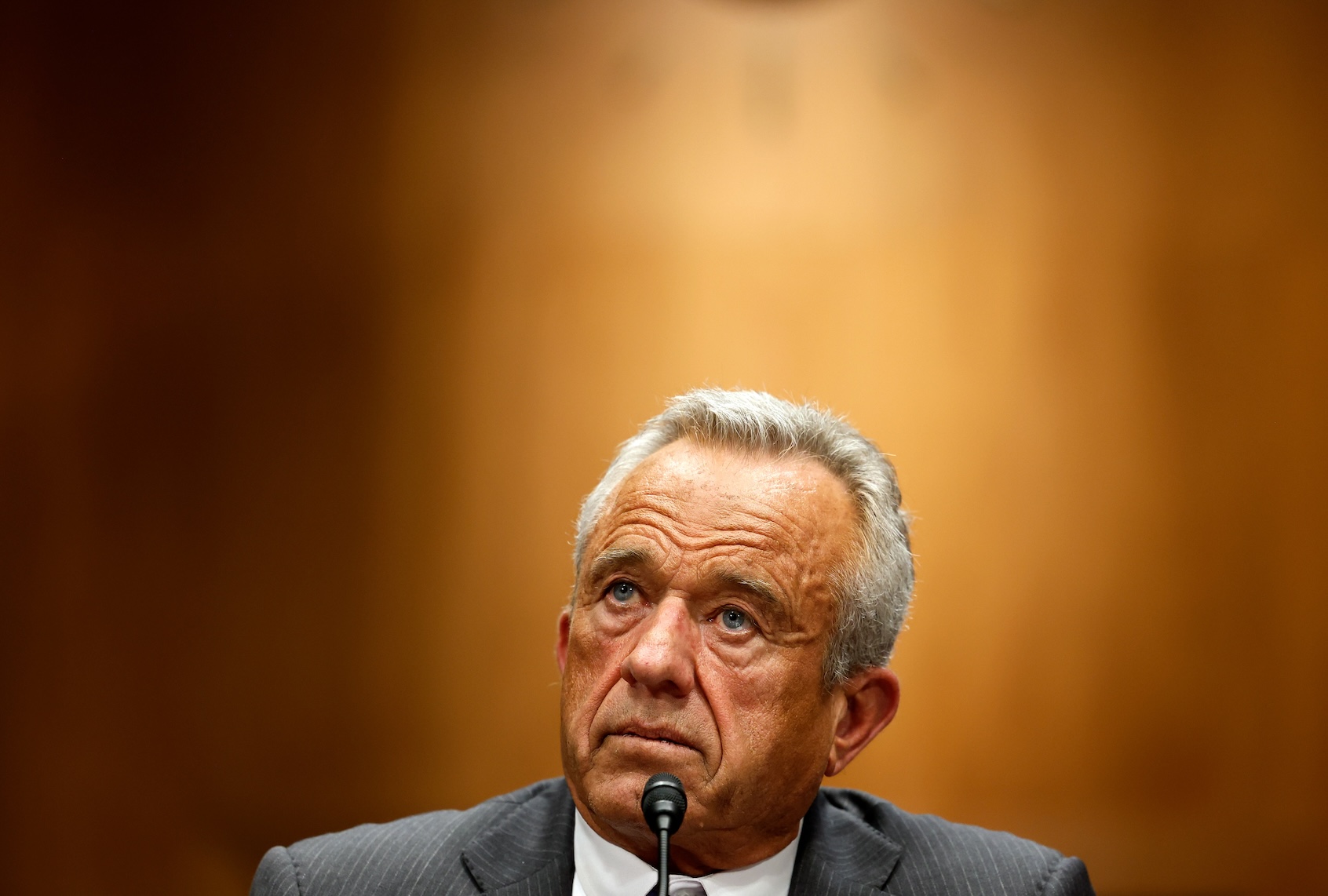
But public trust in the U.S. Center for Disease Control and Prevention (CDC) is declining, and no such similar call to action has been made. Meanwhile, surveillance of the virus has been lacking. During the record-breaking government shutdown, the CDC stopped updating key dashboards tracking influenza, RSV and COVID-19 activity. While tracking resumed after the shutdown, some public health experts aren’t confident that a tough season will be well-managed by the public health agency under Health and Human Services Secretary Robert F. Kennedy Jr.’s leadership.
“I am concerned about everything related to infectious disease under the Trump administration because the chief of HHS is an anti-vaccine advocate and doesn’t even believe in the germ theory of disease,” Dr. Amesh Adalja, an infectious disease expert and senior scholar at Johns Hopkins Center for Health Security, told Salon. “He has destroyed the CDC.”
Katelyn Jetelina, an epidemiologist and author of the newsletter Your Local Epidemiologist, told Salon, that it’s important to note that states still collect data to send to the CDC.
“Within CDC, there is an important distinction between political operatives and CDC scientists,” Jetelina said. “The scientists are still in control of the data.”
But streams of data are thinner, Rajnarayanan noted, and more delayed because of the shutdown.
We need your help to stay independent
Despite the mutations, Adalja said getting vaccinated is still the best way for people to protect themselves against the flu this season because the vaccine contains three strains. While it’s a “mismatch” for the H3N2 strain, it’s still protects the H1N1 or influenza B components.
“The dominant H3N2 strain has evolved away from the H3N2 included in the vaccine so the vaccine strain is not perfectly matched to it,” Adalja said. “The influenza vaccine remains the best way to protect oneself from the virus, especially against severe disease.”
Rajnarayanan said while masks are “not popular in the USA right now,” they are still a good option for protection.
“Stay home when sick and seek early testing and antivirals if you’re high-risk and develop symptoms,” he said. “Layering these simple measures will significantly reduce transmission and protect the people most likely to become seriously ill.”
Read more
about public health