On Nov. 12, 1998, a week before her sixth baby was due, Holly's nurse-midwife agreed to induce her labor. While there were no medical reasons for induction -- one of Holly's five daughters had weighed 9 pounds 4 ounces and had been born after only five minutes -- the nurse-midwife contends that Holly complained of being tired of being pregnant. Before consenting to the induction, Holly's midwife says, she asked one of the obstetricians in her group practice if Holly would be a good candidate to try a new induction drug. He approved the prescription.
Holly disputes her midwife's story, asserting that the midwife recommended induction against Holly's better judgment. "My body was made to have babies," she told me. With five vaginal births to her credit, Holly had confidence in her ability to labor.
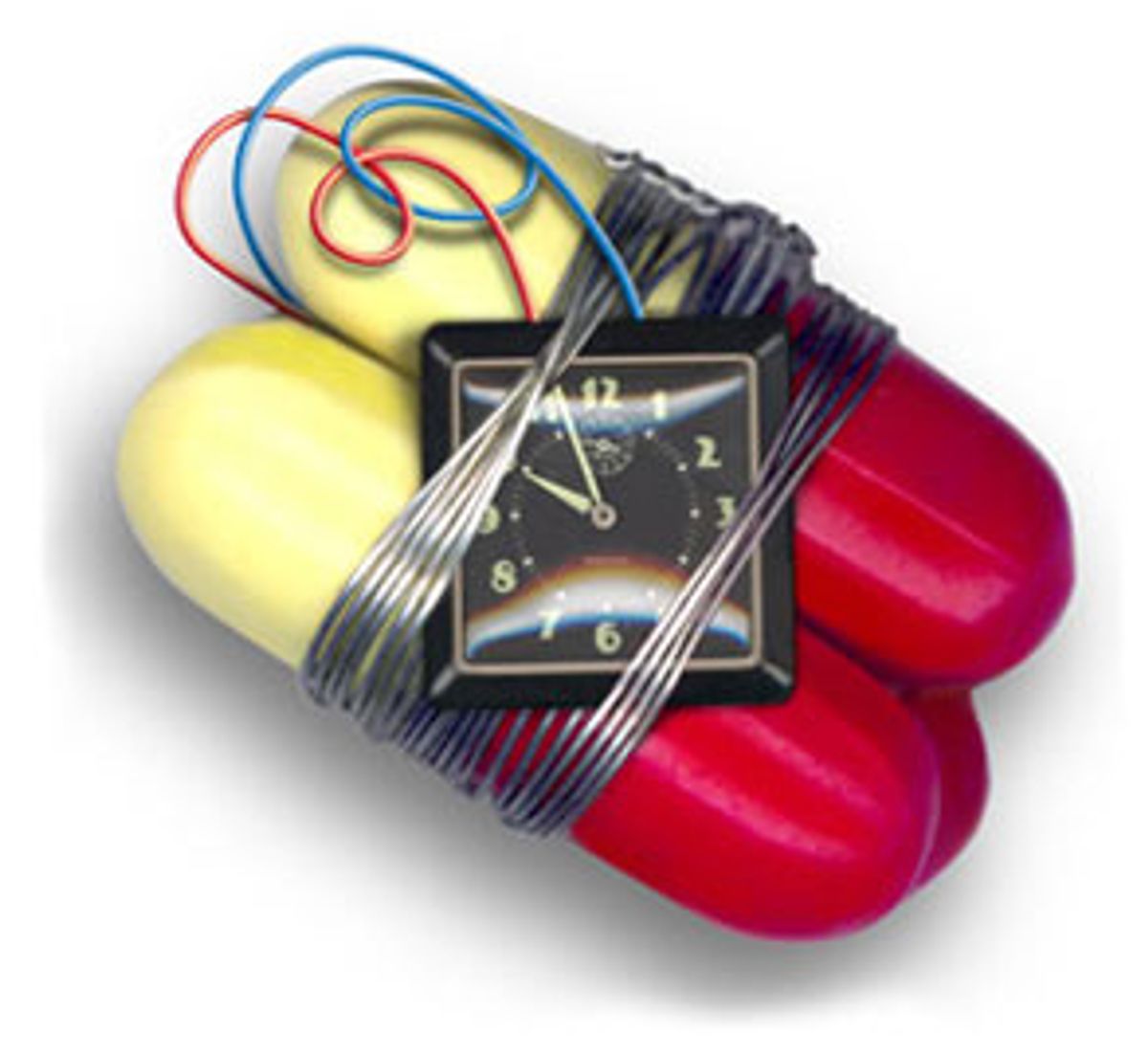
Whatever the truth, both parties agree that over the next several hours the nurse-midwife gave Holly three 25-microgram doses of Cytotec. (Because of legal considerations, both parties requested anonymity.) What Holly didn't know and the midwife never told her was that it was an unapproved drug with potentially disastrous side effects.
One hour after the third dose, labor began, with contractions every two and a half minutes. According to Holly's 19-year-old daughter, Ann, who was present throughout labor, Holly handled herself very well.
Thirty hours later, her cervix not yet fully open, Holly stood up and walked around. Then her bag of water broke. A little later she heard a popping sound from her body. The midwife monitoring her labor noticed that the baby's heart rate had dived from a normal 130-140 beats to a frightening 40 beats per minute.
She exhorted Holly to push, and within five minutes, Holly's 8-pound, 13-ounce daughter was born, followed by a huge gush of blood. The baby was blue and didn't breathe on her own, so the resuscitation team intubated her.
Holly, meanwhile, continued to bleed. Frightened, she told her midwife that something was wrong. The midwife assured her that her blood loss was not enough to warrant a doctor's presence. Later, realizing that Holly was bleeding excessively, the midwife removed several huge clots from her vagina, gave her medication to stop the bleeding and left her in the care of nurses.
Ann and Darryl, Holly's husband, were far from reassured. By this time, Holly lay unconscious, white as a ghost. They helplessly watched her struggle for breath. Darryl begged the nurses to get a doctor and the midwife directed a nurse to call for a doctor on the intercom. The physician who entered the birth room two minutes later was shocked at Holly's condition. "This lady is dying," he shouted. "I'm taking her to the O.R.!"
Holly's heart stopped twice during the surgery. At one point, the doctor told Darryl that he did not expect her to survive. Her uterus had ruptured from the top down through the cervix. This kind of wound is characteristic of Cytotec-related ruptures, according to obstetricians I've since spoken to. (One doctor described them to me as "totally exploding.") Surgeons removed Holly's uterus along with one of her ovaries and a fallopian tube. Thirty-seven units of blood, plasma and platelets were required to replace the blood lost during her ordeal. Gone forever was her chance to have another baby.
Was Holly's labor a nightmare fated to happen, with or without intervention? Or did Cytotec cause her uterine rupture, thereby threatening her and her daughter's life? As with so many forms of obstetric intervention, even hindsight isn't 20/20. Every birth is unique, and the influences on labor are far more numerous than most studies can account for. And even with large, long-term, controlled studies, it is sometimes complicated to ferret out the facts about the efficacy or safety of a given medical procedure.
Cytotec, however, doesn't have the benefit of such scientific debate, because it is still essentially an experimental birth drug that is being tested ad hoc by trial and error. But most patients are never informed of this fact.
As a midwife of 30 years and one of the founders of the natural childbirth movement, I have overseen more than 2,000 births at my birthing center in Summertown, Tenn. Over the years I've listened to innumerable anecdotes about the dangers of medical intervention. But the stories I was hearing about Cytotec I found especially unsettling.
Over the past three years I have watched in increasing dismay as this once little-known ulcer medication has become a popular obstetric drug -- one with potentially horrifying side effects and a frightening lack of safety protocols. Buried in study after study, reports show that the drug has been connected to numerous cases of ruptured uteri and even a few maternal deaths, stillbirths and newborn deaths. Despite these reports, however, tales like Holly's -- in labors attended by practitioners who appear to have little understanding of the drug's potential dangers -- continued to reach me. In fact, the widespread use of Cytotec essentially amounts to a massive medical experiment carried out on thousands of unsuspecting women -- a situation, sadly, that is all too common in the world of modern obstetrics.
Most Cytotec-induced labors do not cause adverse effects like those in Holly's labor -- in fact, for a significant number of women Cytotec seems to work amazingly well. In a way, that's what scares me the most. Since it works so efficiently for a majority and can be prescribed obstetrically without Food and Drug Administration approval, there's less motivation for learning why for some women the drug has a catastrophic effect. Aside from the oft-cited though widely ignored warnings against giving it to women who have had Caesarean sections, we know very little about which women are at risk.
What we do know about Cytotec is that it is dirt cheap: A single 25-mcg dose costs roughly 13 cents; Pitocin, in contrast, necessitates hundreds of dollars in high-tech intervention. Since Cytotec is made in 100-mcg tablets to be taken orally, its quarter-tab dosages are necessarily inaccurate: Nurses or doctors have to literally cut up the pills with little knives. Furthermore, there is still no agreement as to the dosage size or interval or even most appropriate route of administration. The most common means of administration, by placing a quarter-tablet next to the cervix, is so easy that some doctors and midwives give the pills to women to take home and insert themselves. As a result, some women who experience emergency complications like Holly's do so without a hospital staff to care for them.
Unlike a Pitocin drip, which has a half-life in the body of about 10 minutes and can easily be turned off if the woman responds to it violently, once Cytotec is administered, you can't get it out and nobody knows its half-life. This gives Cytotec an unpredictable, stealthy quality. Sometimes even when it is doing serious damage to the uterus, the woman has no awareness that something's wrong; other times it creates immediate violent contractions. Moreover, the ruptures can occur many hours after a single dose in which the drug seemed to have caused no adverse effects. No one understands how this works, but it has been the subject of discussion both in the medical literature and in physician chat rooms.
Finally, in an era of managed-care obstetrics in which doctors are seeing patients in their offices at the same time that they monitor other women's labors across town in the hospital by telephone, Cytotec's great claim to fame -- prompt, timely labors -- is a phenomenal boon. In most cases an obstetrician must be present at the time the baby is born to be paid in full for a birth. So financial factors may influence some doctors to induce labor at a convenient time. Moreover, most cases of malpractice litigation involve situations in which doctors were not present and an adverse outcome occurred. Hence doctors have ulterior motives for using drugs like Cytotec, which help speed labor and thereby ensure that they won't miss the big event.
How many women are being given Cytotec? Marsden Wagner, a Washington, D.C., perinatal epidemiologist, estimates that every year at least 150,000 U.S. women (about 3 percent of all births) are given Cytotec to start labor. But based on my conversations with other doctors and nurses, I sense that the number may be much higher. Its usage is certainly growing rapidly. Wagner also notes that the Oregon State Health Department recently told him that Cytotec is now the state's most common method of induction.
How did Cytotec become so widely used and yet remain so underresearched? In 1992 and 1993 the first reports of the obstetric use of the small white tablet -- generically known as misoprostol -- indicated that it could be highly effective for starting labor in women, whether or not their cervixes were ripe. (In contrast Pitocin, the most common induction drug, often doesn't work unless the cervix is already primed and therefore affords doctors fewer choices.) Cytotec had already been used in combination with other drugs as a chemical abortive -- why not use it as an induction medicine? Lacking other information, many physicians began incorporating it into their practices.
A few years passed before the first published reports appeared detailing Cytotec's adverse effects on labor induction. By then, word of mouth in medical circles had made Cytotec the new darling of American obstetrics. Cost-effective, quick and easy to administer, Cytotec was fast becoming a popular alternative to Pitocin, which requires a full high-tech approach, including I.V., continual fetal monitoring and often (because of its reputation for triggering especially painful contractions) an epidural. Cytotec, in contrast, can be administered (though it shouldn't be) in virtually any setting.
Just how many women have been hurt by Cytotec? The question is nearly impossible to answer. No one has done large-scale studies of the drug, and the doctors and midwives who administer it do so with such vastly different protocols that mixing and matching results from various studies would not render reliable data. The most rigorous scientific authority in English on the effects of healthcare, the Cochrane Library, cautions that too few well-designed studies have been carried out to assess the risk factors associated with using Cytotec for labor induction. While conceding that Cytotec is more effective than conventional methods of cervical ripening and labor induction, it cautions that "the apparent increase in uterine hyperstimulation is of concern."
Unable to find large-scale, comprehensive reporting on obstetric use of the drug, I decided to do a little statistical sleuthing (however unscientific) on my own. My research, and my gut sense, based on years of experience as a midwife, indicate that there are significant risks associated with Cytotec, certainly higher risks than those associated with other forms of induction like Pitocin. Combining the results in 20 studies of Cytotec-induced labors published in peer-reviewed journals and papers presented at professional meetings -- a total of 1,958 births -- I discovered a total of two maternal deaths, 16 baby deaths, 19 uterine ruptures and two life-threatening hysterectomies.
To make sense of these figures, consider the normal incidence of uterine rupture, the most common serious side effect of Cytotec. Uterine rupture virtually never occurs in spontaneous (unaugmented) labor in women who've had no previous uterine surgery. Probably because of differing practices surrounding labor induction and augmentation, the rate of uterine rupture varies widely from hospital to hospital. Uterine rupture is less likely to happen in an out-of-hospital birth. Most midwives providing these services do not use drugs to augment labor. The complication has been reported as frequently as one in every 100 births and as rarely as one in every 11,000 births. In my own group practice at the Farm Midwifery Center in Summertown, Tenn., in approximately 2,100 births we have had no uterine ruptures.
By contrast, approximately one in 100 Cytotec-induced births in the 20 studies I looked at resulted in uterine rupture. About half occurred in women having vaginal birth after Caesarean, the others among women who had had no previous uterine surgery.
In fact, it is women who have had Caesareans who are at greatest risk from Cytotec. An article published in 1999 in the American Journal of Obstetrics and Gynecology reported that uterine rupture occurred in five of 89 women with previous Caesarean delivery whose labors were induced with Cytotec -- about one out of 16, a shockingly high figure, representing a more than 28-fold increase over those who did not have Cytotec induction for VBAC (vaginal birth after Caesarean). One of the five ruptures also caused a baby to die.
According to epidemiologist Wagner, "It can be reliably estimated that between 1990 and 1999, as a result of the widespread off-label use of Cytotec for vaginal birth after Caesarean section, well over 3,000 women in the United States suffered a ruptured uterus, resulting in at least 100 dead newborn babies."
Amniotic fluid embolism, or AFE, is perhaps the most frightening complication associated with powerful labor-inducing drugs like Cytotec and Pitocin. AFE, which occurs when the amniotic fluid enters the mother's bloodstream, is one of the most dangerous complications that can happen in birth. More than 60 percent of women and their babies die when it occurs, with survivors usually suffering neurological impairment.
The rate of occurrence of AFE, once thought to occur only once in 80,000 births, seems to be rising in the United States. Chicago writer Deanna Isaacs, whose daughter died from AFE in 1994, found that the incidence of AFE at the Phoenix, Ariz., hospital where her daughter died in labor was 1 in only 6,500 births. AFE is now one of the leading causes of maternal death in the United States. Two cases of fatal AFE are associated in the medical literature with the use of Cytotec; a midwife told me about a third.
Alarmingly high as these figures are, they almost certainly don't reflect all of the adverse outcomes associated with Cytotec. I also gathered information -- much of it hair-raising -- from Internet chat-room discussions involving physicians who signed their names to their comments, as well as from obstetricians and midwives. This is anecdotal evidence, yes. But we can't afford to ignore anecdotes because current medical studies are inadequate, the drug has not been subject to FDA approval and mothers' and infants' lives are at stake.
The enthusiastic discussion of Cytotec in medical chat rooms sheds light on why the drug has become so popular in the United States. "You can almost count on a delivery 12 hours after inserting the Cytotec tablet," said one doctor. Another doctor added a cautionary note: "I must say that I have heard some great things about Cytotec myself. I know some people who have used it and say that they have pretty good luck with it. It sounds like your ladies are pretty happy with its effects -- two-hour labors and such. Just be careful. I would have to say that the biggest danger is leaving the woman alone. The stuff turns the cervix to complete MUSHIE [emphasis in original] and opens it with a couple of contractions. So whatever you do, remember that you must not stay gone too long."
Over the past 30 years, I have watched as wave after wave of medical fads have washed over the institution of modern childbirth. But one thing, unfortunately, hasn't changed: The push to discover a panacea to cure the pain and inconvenience of childbirth drives doctors to experiment -- and the women are usually the last to know.
In this case, to be sure, the demands of the women themselves are part of the problem. The Cytotec controversy is inextricably tied up with the increasing rate of induced labor in the U.S. Until fairly recently, induced labors were fairly rare: Now, one birth in five is induced, with only a small percentage of these inductions being medically necessary. Harried doctors in the HMO age are driving some of this, but women, too, are demanding faster labors. (This is not surprising, considering that the United States has the shortest maternity leave in the industrialized world.) If this trend increases, we can expect to see an accompanying rise in the medical problems that result when the strongest muscle in the human body -- which is also paper thin -- is stimulated to contract violently.
How was it that Cytotec came to be used as an obstetric drug in the first place? Misoprostol was originally developed by G.D. Searle & Co. of Chicago to prevent gastric ulcers in people who take anti-inflammatory drugs such as aspirin for arthritis pain. In 1988, it was approved by the FDA solely for this use. Yet it is quite legal for physicians to prescribe drugs for indications other than those for which the drug has received FDA approval.
This common practice, known as "off-label" use, usually involves prescribing one drug for another purpose. (Incidentally, no such loopholes exist for the use of pharmaceutical drugs in most Western European countries.) With misoprostol the practice seems particularly egregious: taking a medication meant for oral ingestion and inserting it vaginally.
According to Claudia Kovitz, public affairs specialist for Searle, the company does not intend to apply for FDA approval of Cytotec's use in starting labor. Indeed, why should it? At 13 cents a dose, with women taking no more than three doses per birth, the drug is too cost-effective to waste a heap of money on research whose primary result might only be to make the drug illegal to prescribe.
So what protection do pregnant women have when it comes to drugs that are prescribed for another purpose? Very little, according to Laura Bradbard, spokeswoman for the FDA. "People think we have more authority than we have. We approve a product for a particular indication, based on the data we receive. A physician is free to use a drug for any use he or she feels will benefit a patient. There are no safe drugs. You need to do your homework, ask a lot of questions and speak with your physician about your case and the medications," Bradbard said.
And even when the FDA approves a drug, there are no guarantees. "Once a drug reaches the marketplace, that's when we find out all the adverse events, because we have only seen it in 3,000 to 6,000 people perhaps," said Bradbard. "Then it goes into the marketplace, where you have a million prescriptions. Then a reporter will say to me, 'You are approving things too fast. You didn't find it.' Well, we can't find it. It's mathematically impossible. We have to have it in the marketplace and then we have to make warnings."
But Holly and her husband, like most patients who receive Cytotec, never received any warning. "We didn't know it wasn't FDA approved," she said. "We would have never let them use me or my baby as guinea pigs."


Shares