If you could wander inside your own lungs from a microscopic vantage point, it would seem like a horror-fantasy universe straight out of Guillermo del Toro or H. P. Lovecraft.
“There is a ‘lung microbiome’ which also depends on mucus alterations.”
As you wander through the tubes of your upper and lower respiratory tract, you’d be surrounded by mucus and hair-like structures known as cilia. These millions of cilia exist to filter out tiny harmful particles, making up “a complex branching network whose surface nears 100 meter squared,” as Alexandre Persat, a Swiss scientist at the Global Health Institute at École Polytechnique Fédérale de Lausanne (EPFL), puts it.
Yet the wondrous complexity of the human airway also makes these organs frustratingly enigmatic. Among other challenges, it is difficult to realistically recreate their conditions in experiments.
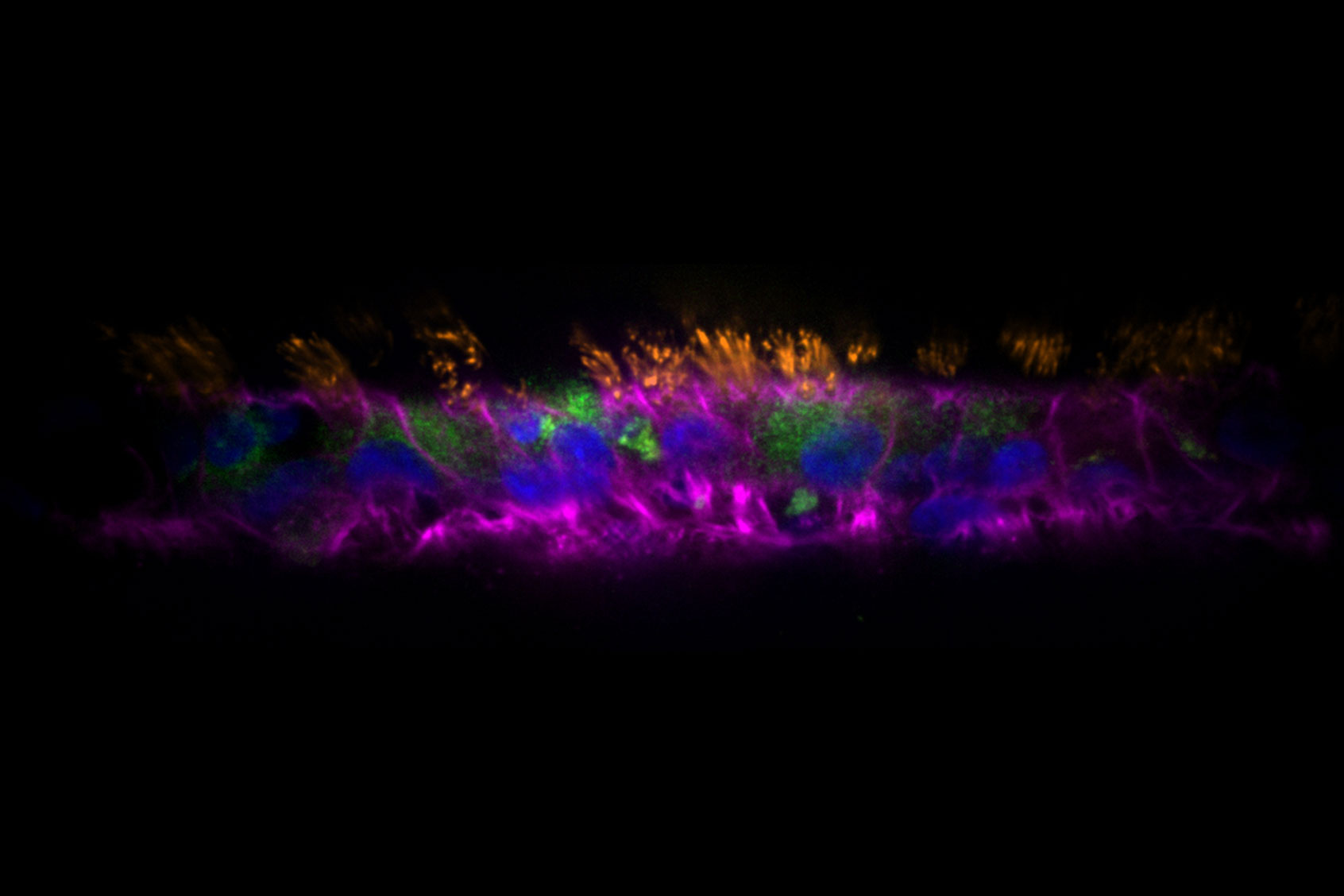
That is, until now. In a recent study published in the journal PLOS Biology, a team led by Persat,developed special organoids, which are miniature tissues grown from stem cells that resemble actual human organs and tissues. Known as AirGels, they can help researchers fight biofilms, or colonies of bacteria that are highly resistant to medications and the immune system.
These aren’t the first organoids — indeed, years ago scientists developed some to resemble other organs, like the brain — but these are the first organoids that work like the human respiratory system. For this design, they targeted Pseudomonas aeruginosa, a nasty bacterium associated with deadly diseases like hard to treat forms of pneumonia and sepsis syndromes.
“Despite extensive in vitro experimentation, how P. aeruginosa forms biofilms at the airway mucosa is unresolved,” the authors of the paper explained. Using their AirGels, however, the scientists investigated the role mucus plays in P. aeruginosa biofilm creation under conditions similar to those in living human lung tissue. In fact, it was revealed that the bacterium exploits the body’s own mucus production, giving it the advantage it needs to colonize the human airway. The authors concluded the same mucus which captures pathogens, or dangerous disease-causing substances in our bodies, has a downside.
“Our results therefore suggest that, while protecting epithelia, mucus constitutes a breeding ground for biofilms,” they explain.
Want more health and science stories in your inbox? Subscribe to Salon’s weekly newsletter The Vulgar Scientist.
“Our results therefore suggest that, while protecting epithelia, mucus constitutes a breeding ground for biofilms.”
These discoveries could save millions of lives, as the pathogen that the scientists targeted is devastatingly common.
“Pseudomonas aeruginosa lives predominantly in soil where it competes with many other microbes and predators,” Persat told Salon by email. “They can infect any organism and commonly contaminate hospital environments. As a result they are a leading cause of nosocomial infections, in particular at the ICU.”
In addition to colonizing the lungs of patients using ventilators, the bacterium is especially dangerous for cystic fibrosis patients.
“We found that the mucus is the major substrate for these biofilm,” Persat explained. “There is a ‘lung microbiome’ which also depends on mucus alterations. In the context of infection, there are multiple pathogens involved, which can also include viruses. That’s quite common in cystic fibrosis, but it also happens to us with a virus infecting us while we are taking antibiotics.”
Even with this latest study, scientists still have a lot to learn about the role of the lung microbiota in infections.
“The number of commensal bacteria in very low compared to the gut so it is possible that they don’t do much,” Persat said. “Conversely, it is possible that pathogens also compress intestinal mucus in the gut to promote infection.”
Either way, Persat hopes that scientists can use AirGels going forward to research all kinds of respiratory diseases, as well as crack the mysteries of how the little universes inside our airways both help and harm our health.
We need your help to stay independent
“Organoids have a very strong potential in fundamental research to understand infections, because they allow us to replicate critical parameters of specific tissues like gut and lung,” Persat told Salon. “They also allow us to perform high resolution measurements such as microscopic imaging and gene expression. At the same time, organoids change our perspective on animal experimentation, because they replicate aspects of human physiology much better than a mouse or a rat.”
He concluded, “I think they will revolutionize the way we study infections and microbiota. Our lab is pushing to democratize their use to enable the discovery of new drugs against antibiotic resistant pathogens.”